Introduction
1. DEFINITION
According to the definition of the European Academy of Allergy and Clinical Immunology (EAACI) [1], the following classification structures the variety of adverse food reactions: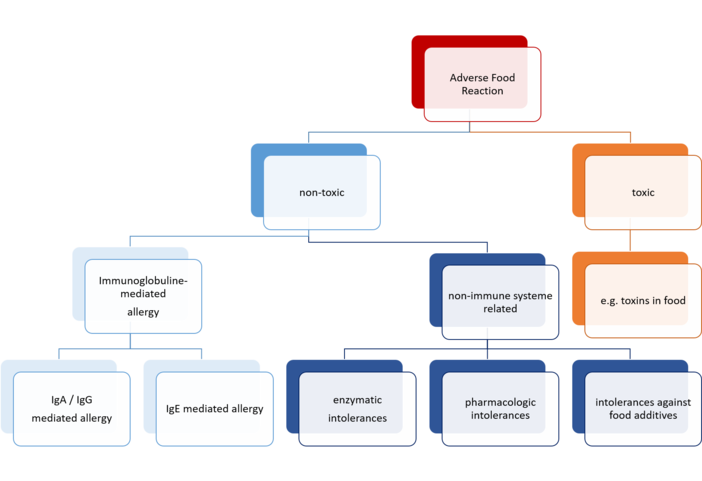 Fig. 1: Pathophysiological classification of adverse food reactions
Fig. 1: Pathophysiological classification of adverse food reactions
In a more restricted definition, the term adverse food reaction is used synonymously to food intolerance and means incompatibility phenomena with no toxic or allergic reaction [2] [3] [4]. The WHO classification ICD-10 distinguishes between the following categories:
| ICD-10 Code | Description |
|---|---|
| A05 | Bacterial foodborne intoxication, unspecified |
| L27.2 | Dermatitis due to ingested food |
| T78.0 | Anaphylactic reaction due to adverse food reaction |
| T78.1 | Other adverse food reactions, not elsewhere classified |
| E70-E90 | Metabolic disorders |
| K90.0 | Coeliac Disease |
2. EPIDEMIOLOGY
It has been estimated that about 1-2 percent of all people suffer from adverse food reactions. In contrast to this figure, 10-20% of people say that they are self-aware of food intolerance. [5]
3. PATHOPHYSIOLOGY
3.1. Toxic Reactions
Toxic reactions after food intake are due to the toxicity of distinct food ingredients.
3.2. Non-toxic Reactions
Non-toxic reactions are based on an individual sensitivity of an organism to specific food ingredients. There is a common distinction between immunoglobulin-mediated and non-immunological reactions.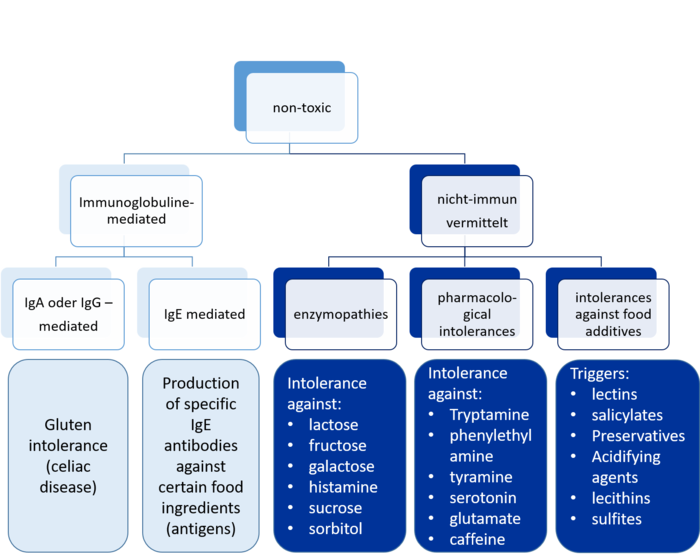
Fig. 2: Pathophysiological classification of non-toxic adverse food reactions
3.2.1. Immunological Reactions / Food Allergy
A food allergy is an abnormal immune response to food. The signs and symptoms may range from mild to severe. They may include itchiness, swelling of the tongue, vomiting, diarrhea, hives, trouble breathing, or low blood pressure. This typically occurs within minutes to several hours of exposure. When the symptoms are severe, it is known as anaphylaxis. According to the underlying pathomechanisms, two forms are distinguished:
- IgE-mediated reactions
- non-IgE-mediated reactions (IgA or IgG): e.g. gluten intolerance (Celiac Disease) is one of the immunologically induced non-IgE-mediated food intolerances.
3.2.2. Non-Immunological Reactions
According to the underlying pathomechanisms, the following types of adverse food reactions without toxic or allergic background can be distinguished:
Resorption-linked intolerances (transporter defects)
Resorption-linked intolerances are due to a diminished or complete loss or functional transporters, which renders resorption of certain food ingredients or metabolites impossible for the persons affected. The transporter defects can be either congenital or acquired, e.g. in the case of fructosemal absorption (intestinal fructose intolerance).
Enzymatic intolerances (enzymopathies)
The underlying cause of enzymopathies are distinct enzyme deficiencies or malfunctions that make digestion of certain food components impossible for the persons affected. The enzyme deficiencies or malfunction can be either congenital or acquired. The following enzymopathies are known:
- lactose intolerance
- hereditary fructose intolerance
- galactose intolerance (see also galactosemia)
- histamine intolerance
- sucrose intolerance
- sorbitol intolerance.
Pharmacological food Intolerances
Certain substances in food are pharmacologically active and – when consumed in large quantities – can lead to symptoms of food intolerance (relative intolerance):
- biogenic amines (tryptamine in tomatoes, phenylethylamine in chocolate, tyramine in cheese and chocolate, serotonin in bananas and nuts)
- caffeine
- glutamate (glutamate intolerance).
Pseudoallergic reactions to food additives
Pseudoallergies show the same clinical symptoms and features as allergies. In the case of pseudoallergic reactions a non-specific activation and degranulation of mast cells occurs.
Typical triggers are:
- Lectins (e.g. in beans)
- Salicylates (e.g. in apples or apricots, but also the acetylsalicylic acid used in painkillers)
- Preservatives (e.g. benzoic acid)
- Acidifying agents (e.g. citric acid, acetic acid)
- Certain medications
- Dyes (e.g. tartrazine)
- Emulsifiers (e.g. lecithin)
- Sulfites.
4. SYMPTOMS, THERAPY AND PREVENTION
In humans food intolerances usually manifest themselves by irritation of the skin and / or mucous membranes. However, lung, gastrointestinal system (20%) and cardiovascular system (10%) may also be affected. The main symptoms are [6]:
- Itching, flush, urticaria, quincke edema
- rhinoconjunctivitis, hoarseness, cough, asthma
- Itching and swelling of the oral mucosa or larynx
- nausea, vomiting, colic, diarrhea
- tachycardia, hypotonia, extrasystole
- inflammation of atopic dermatitis.
Prevention and therapy of adverse food reaction can and should be achieved by avoiding the food triggers in question.
5. SOURCES
[1] C. Bruijnzeel-Koomen, C. Ortolani, K. Aas, C. Bindslev-Jensen, B. Björkstén, D. Moneret-Vautrin, B. Wüthrich: Adverse reactions to food. European Academy of Allergology and Clinical Immunology Subcommittee. In: Allergy. 1995 Aug;50(8), S. 623–635, PMID 7503398.
[2] Pschyrembel klinisches Wörterbuch. 261. neu bearb. Auflage. 2007, ISBN 978-3-11-018534-8.
[3] M. Classen, V. Diehl, K. Kochsiek: 14.4.3 Nahrungsmittelunverträglichkeiten In: Innere Medizin. 5. Auflage. Urban & Fischer-Verlag, München 2006, ISBN 3-437-44405-0, S. 1198.
[4] I. Koop, K. Beckh: 4.21 Nahrungsmittelunverträglichkeit, Nahrungsmittelallergie. In: Gastroenterologie Compact. Georg Thieme Verlag, 2002, ISBN 3-13-126311-3, S. 146.
[5] P. Fritsch: Dermatologie & Venerologie fürs Studium. Springer, Heidelberg 2009, ISBN 978-3-540-79302-1, S. 124ff.
[6] P. Fritsch: Dermatologie & Venerologie fürs Studium. 2009, S. 124ff.
Structure and text passages from Wikipedia
